Dysbiosis: Is SIBO the Missing Link to IBS & IBD?
Gut health is one of the most overlooked aspects in mainstream Western medicine that the integrative community has long established as a key factor in functional wellness. Issues like ulcerative colitis, inflammatory bowel disease (IBD), Crohn’s, and others can trace their origin to the gut.
What’s one common factor for the disruption of the gut? Dysbiosis, or the imbalance of intestinal flora within your digestive system. And when things get worse, this can turn into SIBO, or small intestinal bacterial overgrowth.
Read on to learn what SIBO is, how it affects chronic illness like IBD and IBS, and most importantly, what you can do about it.
What Is SIBO?
SIBO is an acronym for small intestinal bacterial overgrowth, and is characterized by a dysbiosis in the natural gut microbiome within different parts of the digestive tract (1).
You’ve probably heard before that your gut is home to both beneficial and pathogenic bacteria, and when these bacteria are in balance they help maintain the health of your gut and entire body.
But when there is too much or the wrong type of bacteria present, a state of dysbiosis can occur.
For instance, if bacteria migrate from the colon (large intestine) to the small intestine, or when low stomach acid or poor enzyme secrete reduce digestive motility, bacteria in the small intestine can overgrow, leading to uncomfortable digestive symptoms that don’t resolve with typical remedies.
Let our compassionate and knowledgeable team get to the root your digestive discomfort today–Click to schedule an appointment.
What Causes SIBO?
A host of lifestyle, diet, and environmental factors can trigger SIBO, and these risk factors can activate certain genetic predispositions that trigger further chronic illness.
Migrating Motor Complex – Your Stomach Rumbles for a Reason
In between mealtimes and overnight, a mechanism called your migrating motor cortex works to sweep bits of food particles and bacteria into the lower digestive tract or colon (2). You feel this electrical impulse in terms of grumbling waves coming from your abdomen.
But sometimes, the MMC can fail to work properly, leaving too much bacteria higher up in the digestive tract. Then, bacteria meant to be pushed down into the colon can migrate into the small intestine, where they’re not supposed to be.
These bacteria then begin to eat what you eat, fermenting starches and carbohydrates at a higher rate than normal, and causing you gas, bloating, constipation, and a host of other digestive complaints.
Triggers for SIBO
- Medications that slow digestive motility
- NSAIDS
- Other pain medications like opioids which slow motility
- Stress
- Low thyroid
- Low enzyme production
- Low stomach acid (or long-term use of acid-blocking medication)
- Frequent snacking (resulting in inhibition of the MMC)
In short, anything that negatively affects the normal flow of digestion or motility of food through your body can contribute to dysbiosis if conditions persist.
And studies now suggest that SIBO, or a state of intestinal dysbiosis, is a key trigger for both IBD and IBS and plays a significant role in the development and progression of these two conditions (3, 4).
SIBO and Digestive Disorders
Studies have found that as many as 78% of those with IBS also have SIBO, indicating a strong link between dysbiosis and IBS (3).
A Recent meta-analysis has also shown significant prevalence of SIBO in patients with Crohn’s and Ulcerative Colitis (4).
How does SIBO play a role in the progression and development of chronic conditions like IBS and IBD? First, it’s important to understand the difference between IBD and IBS.
What Is IBD vs. IBS?
IBD and IBS share many common symptoms which can be confusing for many people, but they are very different conditions requiring unique treatment methods. To help you better understand, the main differences between IBS and IBD are as follows (5):
Inflammatory Bowel Syndrome (IBS)
|
Inflammatory Bowel Disease (IBD)
|
How does SIBO play a role in the development of IBD or IBS? Let’s find out..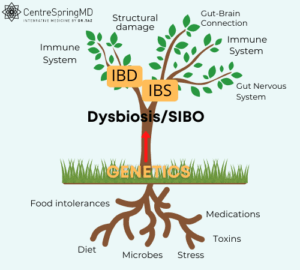
SIBO May Be the Missing Link
Dozens of different lifestyle and dietary factors can trigger states of dysbiosis, as mentioned above. And dysbiosis, when severe enough or when left untreated, can trigger the expression of certain genes which are involved in the progression of chronic digestive diseases such as Crohn’s or IBD.
Even though many digestive triggers (stress, poor diet, etc.) often occur concurrently, usually you can regain balance and avoid full blown dysbiosis with mild adjustment to either diet or lifestyle, and sometimes the trigger is temporary–as is often the case with stress.
When a state of dysbiosis is reached, due to various stimuli combining to overwhelm the delicate microbial balance in your gut–genetic activation and structural damage in the form of inflammation can trigger disease.
How to Know if You Have SIBO
7 Signs & Symptoms of SIBO
- You’re eating a gluten-free diet, but still having symptoms (6). One of the most popular dietary changes is to go gluten-free or grain-free, but when removing gluten doesn’t improve your symptoms at all–something deeper may be going on in your gut.
- Eating more fiber makes your symptoms worse (7). Fiber is a type of prebiotic, which is what living probiotics (or good bacteria) use for fuel. But when you already have an overgrowth of bacteria, fueling their proliferation might make you feel worse.
- Probiotics don’t help either. Similar to prebiotic fiber, your gut may normally need probiotic support, but when you have SIBO, there’s already too many bacteria where they shouldn’t be.
- You’re gaining weight, or losing weight and you don’t know why (8). SIBO can lead to malnutrition and difficulty absorbing nutrients, which can impact weight gain and weight loss.
- You’re exhausted (9). Anemia is one of the symptoms of SIBO. If you have anemia with no known cause, it could be SIBO.
- You suffer with chronic gas, bloating, and digestive discomfort. Contrary to popular belief, these symptoms aren’t normal, especially when they persist.
- Bloating is your normal. After a large meal, or late in the day, your stomach may likely feel and look a little fuller, but uncomfortable bloating after eating especially if accompanied by other symptoms is a sign that bacteria are fermenting foods where they shouldn’t.
Testing for SIBO
There isn’t one single test to diagnose SIBO, but your integrative doctor will most likely do a lactulose breath test or a hydrogen breath test.
These breath tests measure the amount of different types of gases produced by types of bacteria in the small intestine.
Your doctor may also recommend a stool analysis, not to directly diagnose SIBO, but to have a more comprehensive picture of your digestion to pinpoint the root cause of your troubles.
How do you begin treating SIBO? Contact your functional provider.
Treating SIBO with Integrative Medicine
Once your functional doctor has confirmed you have SIBO, he or she will develop a comprehensive plan to restore balance to your digestive system. This may include dietary changes, antibiotics, herbs or supplements, and follow up testing.
Lower carbohydrate diets (like low FODMAP) can help improve SIBO symptoms by removing a substantial portion of the carb fuel bacteria feed on (6).
Foods to Avoid with SIBO:
- Alcohol
- Fermented foods & probiotics
Herbs & Supplements to Help Restore Bacteria Balance:
- Oregano oil
- Garlic
- Berberine
- Biocidin, which contains garlic, goldenseal, and oregano oil, among others.
Getting Bacteria in Check with Your Functional Doctor
Modern lifestyles have made cultivating a healthy microbiome incredibly difficult. And what results is too much of, or the wrong type of bacteria in the wrong place. When left unchecked, this state of dysbiosis can lead to serious problems like SIBO.
Diet, lifestyle, and genetic factors all play a role in maintaining a healthy gut microbiome, and identifying and treating SIBO early is the best way to reverse dysbiosis and restore balance to your gut.
Digestive upset isn’t normal (contrary to popular belief). If your gut is sending you distress signals, don’t wait to contact CentreSpringMD today.
Resources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3752184/
- http://www.vivo.colostate.edu/hbooks/pathphys/digestion/stomach/mmcomplex.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3949258/
- https://pubmed.ncbi.nlm.nih.gov/30735254/
- https://www.crohnscolitisfoundation.org/what-is-ibd/ibs-vs-ibd
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3966170/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5467063/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3099351/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2890937/

