Is It Possible to Have PCOS & Endometriosis?
A significant portion of women with endometriosis also meet the criteria to diagnose PCOS. And according to a 2015 study, the reverse may also be true: Women with PCOS are more likely to be diagnosed with endometriosis (2).
Another study found a strong link between PCOS patients who also experienced chronic pelvic pain and endometriosis (3).
And though endometriosis and PCOS haven’t been considered related to one another, a 2021 evaluation suggests that high levels of androgens and insulin in PCOS could indirectly increase estradiol, potentially increasing endometriosis symptoms, which are worsened by excess estrogen (4).
If a woman has both endometriosis and PCOS, she may experience compounded symptoms and have a more complex path towards healing.
Learn more: Why You Should See a Holistic OB/GYN
Spotting the Differences Between PCOS and Endometriosis
These two conditions, though sharing some common symptoms and demographic prevalence, are distinct in their nature and need for healthcare management.
Symptoms of endometriosis vs. PCOS
Endometriosis and PCOS share some symptoms, like heavy bleeding and struggling to get pregnant, but most of their symptoms are different.
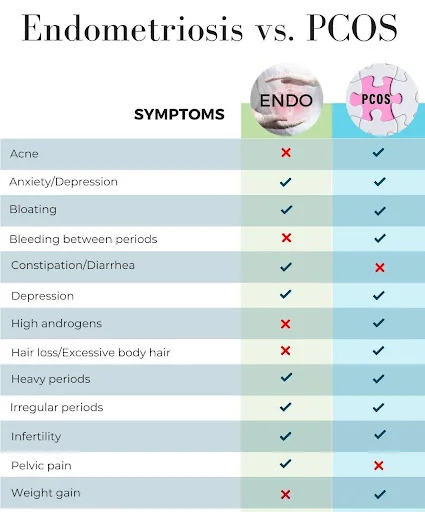
It’s not uncommon for symptoms of PCOS and endometriosis to be misdiagnosed. And, in some cases, symptoms may be subtle or nearly nonexistent. Additionally, not every symptom must be present to have either PCOS or endometriosis.
Underlying Mechanisms
Though they can both cause menstrual irregularities, like heavy or painful periods, and difficulty conceiving, the hormonal issues behind these disorders are very different.
Modern science hasn’t yet determined exactly what causes endometriosis, but there’s a link between toxic burden which affects inflammatory cytokine production, estrogen dominance, and even autoimmunity.
A leaky gut also correlates with endometriosis, and researchers have identified tissue-specific antibodies, indicating that the gut-immune system plays a role in endometriosis (5).
PCOS, according to new research, appears to be caused by metabolic and hormonal misfirings around insulin resistance, as well as excess androgens, and inflammation (6).
Related: PCOS Linked with Critical Nutrient Deficiency
Why It’s Important to Diagnose Correctly
PCOS, with its metabolic implications, can increase a woman’s risk for conditions such as type 2 diabetes and heart disease throughout her life, long after the reproductive years have ended (7).
Endometriosis, with its strong association with inflammation, may possibly increase a woman’s risk for certain cancers often as a result of endometrial hyperplasia. Understanding these implications is crucial for long-term health planning.
Where fertility struggles are concerned, PCOS-related infertility stems from anovulation, or the lack of regular, ovulatory cycles, while endometriosis can interfere with conception due to the inflammatory environment it creates in the pelvic cavity.
Read: PCOS + Endometriosis Increase Risk for Endometrial Cancer
Challenges in Diagnosis and Management
Having both PCOS and endometriosis may make diagnosis more difficult. Symptoms from one condition may mimic those of the other, causing misdiagnosis or delayed diagnosis. Considering that some women already wait 10 years before receiving a proper diagnosis for endometriosis, the potential to further delay treatment is an unfortunate possibility (8).
How An Integrative OB/GYN in Atlanta Can Help
Though there is not yet a complete cure for either PCOS or endometriosis, there are various integrative medicine options available to help manage symptoms and improve quality of life.
Acknowledging the interplay between these conditions is crucial for steering the course of treatment and management. Here, functional and integrative medical professionals can offer a broader toolkit for addressing the multi-faceted nature of PCOS and endometriosis.
The Benefits of a Functional and Integrative Approach
These medical philosophies focus on the root causes of health issues, looking beyond mere symptom management. This approach can be especially beneficial for addressing PCOS and endometriosis, which have complex systemic implications.
Integrative Medicine for PCOS
To manage PCOS symptoms, an integrative team can help you optimize dietary & lifestyle factors based on your genetics and unique biochemical profile.
Whether your goal is hormone balance, becoming pregnant, or better health overall, your CentreSpringMD team will help you manage PCOS in the way that’s best for you.
Integrative Medicine for Endometriosis
Treatment decisions are incredibly individualized and will depend on factors such as your symptoms, stage of the disease, desire to have children, and any personal preferences. Treatment options for endometriosis include:
- Pain management
- Hormone therapy
- Surgery – Laparoscopy to remove adhesions is effective to reduce pain.
- Acupuncture or massage
- Anti-inflammatory diet changes
Read: The Integrative Approach to Endometriosis
What to Remember
For women grappling with PCOS, endometriosis, or a combination of both, the path may seem daunting. But with an engaged integrative medical team, comprehensive support structures, and a commitment to personal health, the destination—relief, fertility, and long-term wellness—is attainable.

