
How Common is Hashimoto’s Syndrome?
Hashimoto’s syndrome is very common, affecting as many as 1-2% of people in the United States. Women are 7-8X more likely to develop the syndrome than men, which may due to differences in hormonal production.
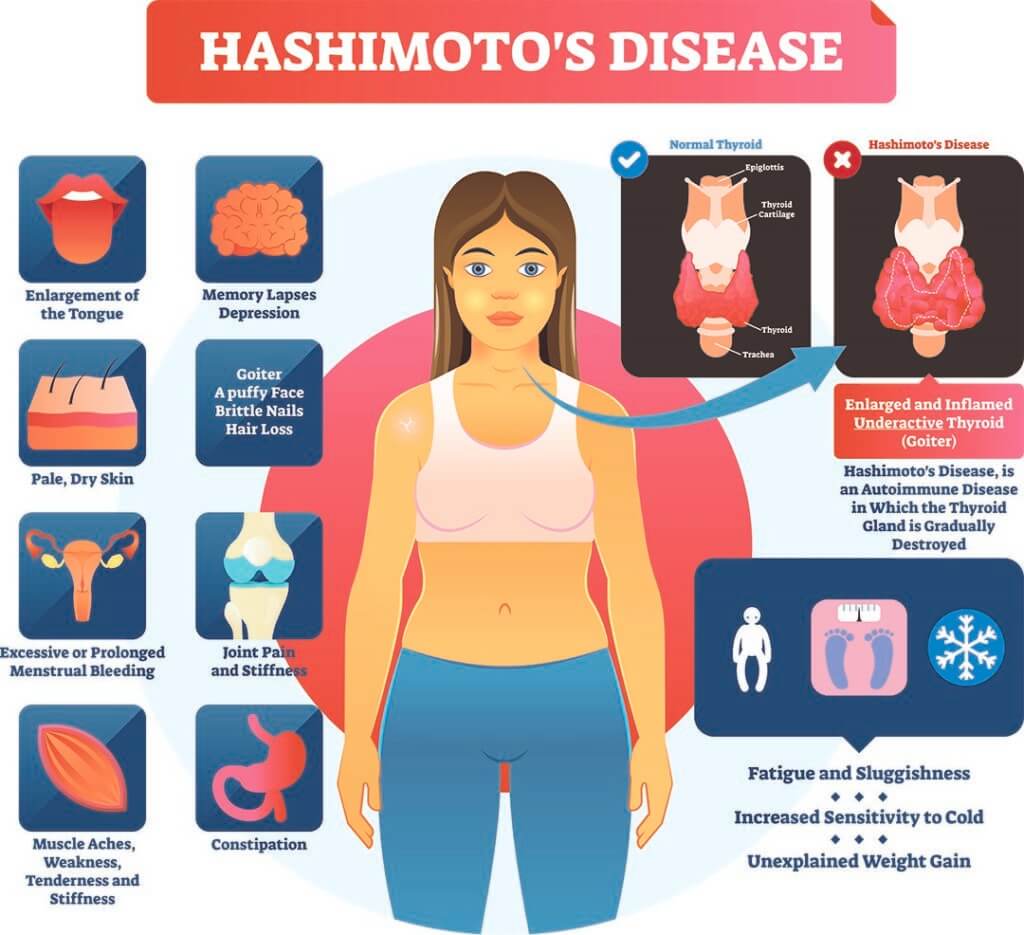
Symptoms of Hashimoto’s Syndrome
Hashimoto’s syndrome is an autoimmune disorder that attacks the thyroid over time. This often causes chronic thyroid damage which typically results in hypothyroidism. Symptoms of Hashimoto’s disease are usually due to the corresponding hypothyroidism (underactive thyroid gland) typical of this condition.
Symptoms:
- Fatigue or Tiredness
- Unexplained Weight Gain
- Constipation
- Increased Sensitivity to Cold
- Muscle Weakness
- Muscle or Joint Aches or Stiffness
- Enlarged Tongue
- Pale or Dry Skin
- Brittle Nails
- Unexplained Hair Loss
- Depression
- Slowed Heart Rate
- Irregular or Heavy Menstrual Periods
- Memory Lapses
Complications of Hashimoto’s Syndrome
Because Hashimoto’s syndrome progresses slowly, many individuals with this condition do not experience symptoms for years. However, left untreated long-term, the syndrome can lead to a number of additional health issues including heart problems, mental health complications, or other diseases.
- An enlarged thyroid, called a goiter, can occur in some cases of Hashimoto’s syndrome. This can often cause visible swelling in the neck area. While the goiter itself is typically not painful or uncomfortable, it can interfere with swallowing or breathing if left untreated.
- Heart Problems. Individuals with an underactive thyroid gland (hypothyroidism), including underactivity due to Hashimoto’s syndrome, can experience higher levels of lipoprotein cholesterol, or “bad” cholesterol. This can result in heart disease including enlarged heart or heart failure.
- Mental Health Issues. Because of the decrease hormonal levels due to Hashimoto’s syndrome, individuals with this condition may experience depression. If Hashimoto’s syndrome is left untreated, this depression may increase over time. Hashimoto’s syndrome can also cause decreased libido and diminish or slow mental functioning.
- In rare cases, Myxedema may occur, which is the escalation of drowsiness and lethargy, followed by unconsciousness. This may be triggered in rare cases in individuals with Hashimoto’s syndrome exposed to cold, sedatives, infection, or other stressors. Myxedema requires immediate emergency medical treatment.
- Birth Defects in Children. Untreated hypothyroidism, including hypothyroidism due to Hashimoto’s syndrome, can increase the risks of birth defects as well as intellectual and developmental problems. There may be a link between hypothyroidism and being born with a cleft palate or a heart, brain, and kidney problems. If you have Hashimoto’s syndrome and are trying to get pregnant or are in the early stages of pregnancy, it’s important to meet with a doctor to discuss treatment.
Causes of Hashimoto’s Syndrome
While the exact cause of Hashimoto’s Syndrome is not known, it is thought that several factors may play a role in the development of this disease, including:
- It often affects people who have family members with thyroid disorders or autoimmune diseases. This suggests that there may be a genetic component to Hashimoto’s syndrome.
- Autoimmune Disorder. Individuals who have other autoimmune disorders such as Addison’s disease, autoimmune hepatitis, celiac disease, lupus, type 1 diabetes, pernicious anemia, rheumatoid arthritis, Sjögren’s syndrome, and vitiligo have been linked to Hashimoto’s syndrome.
- Hashimoto’s syndrome affects as many as 7-8X more women than men, which suggests that sex hormones may play a role in its occurrence.
- While the syndrome can occur even in teenage years or early adulthood, it more commonly occurs in middle-aged patients.
- Radiation Exposure. Individuals who have been exposed to excessive levels of radiation may be at increased risk of Hashimoto’s syndrome.
How is Hashimoto’s Syndrome Diagnosed?
In general, a doctor will test for Hashimoto’s disease if you are tired or fatigued and are experiencing constipation, dry skin, if you have a goiter, or if you have a history of thyroid problems. The diagnosis for Hashimoto’s syndrome usually consists of a hormone test and an antibody test.
Medical History
If you have a family history of Hashimoto’s syndrome, thyroid problems, or autoimmune disorders, you may be at higher risk. Getting your and your family’s medical history can help your doctor assess whether you’re at higher risk for this condition.
Hormone Test
A hormone test for Hashimoto’s syndrome consists of a blood test in which the doctor will look at your thyroid and pituitary gland hormone levels. If your thyroid hormone levels are low, this may be an indication of hypothyroidism, possibly as a result of Hashimoto’s syndrome.
The doctor will also look for increased pituitary hormones. While hypothyroidism can sometimes be caused by a lack of the pituitary hormone TSH (thyroid-stimulating hormone), this is typically not the case in Hashimoto’s syndrome. Instead, with untreated Hashimoto’s syndrome, the pituitary gland often releases additional TSH in an effort to stimulate the thyroid gland to produce more thyroid hormone. TSH levels are used as one of the main indicators for the syndrome, as well as to test the efficacy of treatment.
Antibody Test
As part of the blood test, your doctor may also perform an antibody test. Because Hashimoto’s syndrome is an autoimmune disorder, the presence of antibodies against thyroid peroxidase, an enzyme that plays an important role in producing, would indicate the possible presence of Hashimoto’s syndrome.
Ultrasound
Your doctor may also take an ultrasound of your thyroid. This will confirm that the enlarged thyroid isn’t caused by non-Hashimoto’s syndrome factors, such as thyroid nodules—small lumps found on the thyroid gland. An ultrasound is most commonly ordered if the patient has an enlarged thyroid but is not showing elevated levels of TSH in the blood.
Of the tests used to diagnose Hashimoto’s syndrome, the test for TSH is the most widely used. This is also the test used to measure the efficacy of the hormone therapy used to treat Hashimoto’s syndrome.
Hashimoto’s Syndrome – Hormone Replacement Therapy
At this time, there is no permanent cure for Hashimoto’s syndrome. However, hormone replacement therapy can help regulate hormone levels and help your biological functions and metabolism return to normal.
Most commonly, doctors will treat Hashimoto’s syndrome with hormone replacement therapy. This therapy typically includes the hormone replacement levothyroxine, which is identical to the hormone thyroxine which is normally produced by your thyroid gland.
Initially, your doctor may choose to retest your TSH level every few weeks after your hormone replacement therapy begins to ensure the right dosage. If you have severe hypothyroidism or a heart condition, your doctor may start you with a small dose of hormone replacement medication and will gradually increase the dose over time to give your heart time to adjust to your increased metabolism.
Since hormones regularly fluctuate, it will be important to routinely visit your doctor about every 12 months to check your TSH levels. This will ensure your dosage is still conducive to your current condition.
In addition, your doctor may also prescribe an anti-inflammatory like LDN. Anti-inflammatories like low-dose naltrexone (LDN) help manage inflammation associated with Hashimoto’s syndrome.
Natural Treatments
Hormone replacement therapy is the first line of defense for individuals with Hashimoto’s disease. There is no scientific evidence that natural remedies or lifestyle changes can cure or reverse the effects of hypothyroidism due to Hashimoto’s syndrome. However, some lifestyle changes can help support the function of your thyroid and contribute to your overall recovery plan.
Balancing the Gut Microbiome
Balancing the gut microbiome is important in helping to treat Hashimoto’s syndrome. This is because in an imbalanced microbiome trigger inflammation that drive up antibody levels.
Managing candida, bacterial overgrowth, and parasites are all a part of Hashimoto disease management.
Diets Free from Grains, Dairy, & Highly Processed Foods
While inflammatory foods such as grains, dairy, and highly processed foods aren’t the cause of Hashimoto’s syndrome, they can trigger an autoimmune response. This can exacerbate inflammation and tissue destruction. In these cases, a diet free from grains, dairy, and highly processed foods can be beneficial to individuals living with Hashimoto’s syndrome.
Diets such as paleo or gluten-free diets can be effective for individuals with Hashimoto’s syndrome, as can diets that focus on the following foods:
- Lean Meats
- Fish & Seafood
- Fruit
- Vegetables (avoid starches and excessive cruciferous vegetables)
- Nuts
- Seeds
Iodine
Since iodine is added to table salt in the United States, it’s uncommon for Americans to have an iodine deficiency. However, for individuals with Hashimoto’s syndrome, it can be helpful to be conscious of iodine in your diet. Too little iodine may contribute to goiters while too much can increase the symptoms of hypothyroidism.
Ask your doctor about adding more natural sources of iodine in your diet. Some examples of iodine-rich foods include:
- Seafood
- Dairy Product
- Eggs
- Prunes
Selenium
While the effects of selenium on Hashimoto’s syndrome are still being studied, some individuals living with the disorder experience a decrease in the number of antibodies attacking the thyroid when taking selenium supplements.
Ask your doctor about adding more selenium-rich foods to your diet, including:
- Eggs
- Pork
- Beef
- Chicken
- Tuna & Sardines
- Brazil Nuts
Zinc
While zinc deficits in developed countries are uncommon, in one 2009 study, some individuals with hypothyroidism syndrome saw increased thyroid hormone levels with zinc supplements.
Talk with your doctor about adding more zinc into your diet with foods such as:
- Beef
- Chicken
- Oysters & Shellfish
- Legumes
Living with Hashimoto’s Syndrome
While Hashimoto’s syndrome cannot be cured, with the right hormone replacement therapy and lifestyle changes, individuals can experience relief from many symptoms from this condition.
If you suspect you may have Hashimoto’s syndrome or are experiencing symptoms related to hypothyroidism such as fatigue, dry skin, depression, or constipation, or if you have an unexplained goiter, reach out to the experts at CentreSprings MD. Our integrative, functional, holistic approach can help you get to the underlying issue behind your symptoms and create a holistic approach to treatment.
[book-now title=’Book an Appointment’ url=’https://centrespringmd.com/contact/’]
Frequently Asked Questions About Hashimoto’s Syndrome
What does Hashimoto’s disease do to your body?
Hashimoto’s disease is an autoimmune disease that produces antibodies that attack your thyroid like it would a virus. Over time, this can cause tissue damage in your thyroid. This damage can decrease your thyroid’s ability to produce thyroid hormones, resulting in hypothyroidism. The damage to your thyroid can also cause a goiter, which is the swelling of your thyroid gland. A goiter can make your throat look and feel swollen and can impact your breathing or swallowing. Decreased thyroid hormones also slow the function of your body’s organs, which can decrease your heart rate, cause weight gain, slow your mental functioning, decrease functioning in your intestines (often causing constipation), and more.
What shouldn’t you eat when you have Hashimoto’s syndrome?
While Hashimoto’s syndrome is not caused by a poor diet, eating a diet that avoids inflammatory foods such as gluten, dairy, or highly processed foods can help prevent triggering an autoimmune response in your body, which may exacerbate symptoms. Those with Hashimoto’s syndrome may benefit from avoiding foods such as:
- Gluten
- Grains
- Dairy
- Highly-Processed Foods
What is the difference between Hashimoto’s disease and hypothyroidism?
Hashimoto’s disease is an autoimmune disease in which antibodies attack the thyroid as if it were a virus. Hypothyroidism is a condition in which the thyroid is not releasing enough of the thyroid hormones thyroxine (T4) and triiodothyronine (T3). Because of the damage to the thyroid in Hashimoto’s disease, this disease often leads to hypothyroidism. In fact, Hashimoto’s disease is one of the most common causes of hypothyroidism in the United States. However, other factors such as thyroid surgery, some medications, or postpartum thyroiditis can also cause hypothyroidism.
Can Hashimoto’s syndrome be cured?
There is no cure for Hashimoto’s syndrome at this time. However, hormone replacement therapy can be very effective in reducing the symptoms of hypothyroidism due to Hashimoto’s syndrome, usually helping those affected with the condition “feel back to normal” as long as they continue treatment.
Does Hashimoto’s affect life expectancy?
No. Because Hashimoto’s is very treatable, it doesn’t typically affect your life expectancy. However, left untreated Hashimoto’s can sometimes lead to heart conditions or heart failure. In extreme cases, it can also cause myxedema, a rare but life-threatening condition that includes progressive drowsiness followed by extreme fatigue and eventual unconsciousness. For these reasons, it’s important to see a doctor if you suspect you may have Hashimoto’s syndrome.
How can we help?
Would you like to learn more about Hashimoto’s syndrome or the treatment process? Contact CentreSprings MD to discuss your symptoms and treatment options or book an appointment today.

