What triggers autoimmune disease flare-ups?
Studies suggest flare-ups are primarily the result of psychological and physical stress on the body (1). Moreover, some studies found that a high proportion (up to 80%) of patients reported significant and “uncommon emotional stress” before their initial disease onset.
According to one article, “not only does stress cause disease, but the disease itself also causes significant stress in patients, creating a vicious cycle” (1).
 Stress—whether physical, hormonal, mental, or emotional—and major stress-related hormones are implicated in the development and progression of autoimmune disease. It is presumed that various factors, including poor sleep, diet, illness, major hormone shifts, and climate involve neuroendocrine hormones which lead to immune dysregulation.
Stress—whether physical, hormonal, mental, or emotional—and major stress-related hormones are implicated in the development and progression of autoimmune disease. It is presumed that various factors, including poor sleep, diet, illness, major hormone shifts, and climate involve neuroendocrine hormones which lead to immune dysregulation.
This prolonged immune dysregulation can result in autoimmune disease, or the worsening of symptoms (such as during a flare-up) by changing or amplifying inflammatory cytokine production.
If it’s time for a little stress relief, our integrative spa has all the relaxing solutions you’re looking for.
Women are more susceptible
Notably, 80% of all those who experience autoimmune disorders are women, raising important questions about genetic and other factors involved in the development of autoimmune conditions (2).
Flare-ups may also be caused or worsened by certain foods that can cause inflammation in the body, including processed sugars and carbohydrates, artificial sweeteners, wheat products, factory-farmed meats, and dairy with hormones (3).
Learn more: Integrative Women’s Health at CentreSpringMD
Common triggers of a flare-up
Good and bad stress
Anything which places stress on the immune system has the potential to trigger a flare-up. Even good stress like traveling or getting married could put your body under additional strain, especially if you are already experiencing symptoms of an autoimmune disease.
Studies indicate travel is one of the top triggers for flaring up symptoms because it often means changing eating habits and routines (4). The natural reaction to changes in routine is stress on the body, which could worsen autoimmune disease symptoms. In addition to travel stressors like adjusting sleeping patterns or dietary restrictions, simply the logistics of getting to your destination can also be stressful.
Changes in season
The seasons can have a huge impact on how well your immune system is working to keep you healthy. For example, the natural change in weather may cause joint pain for those who suffer with rheumatoid arthritis, or difficulty breathing for those with Hashimoto’s thyroiditis.
Gut dysbiosis or SIBO
An unhealthy gut microbiome can lead to an autoimmune flare-up. Small Intestinal Bacterial Overgrowth (SIBO) is a condition in which natural bacteria found in the intestines thrive and grow out of control, causing bloating and other uncomfortable side effects.
 Gluten
Gluten
For those with Hashimoto’s and gluten intolerance, eating foods containing protein can set off a cascade of inflammatory reactions in your body.
Sugar and Dairy
It’s not a hard rule to avoid sugar and dairy, though these are two common foods that can trigger inflammation which results in an increased risk for an autoimmune disease flare.
Seasonal illness or the flu
When your immune system is fighting a virus like the flu, autoimmune disease symptoms can worsen because your body is under additional strain.
Read more: Preparing for Cold + Flu Season
Intense (or too much) exercise
Certain people may need to be mindful of certain types of exercise with an autoimmune disease. Overtraining or participating in endurance activities may exacerbate some autoimmune diseases more than others (5). A high-intensity workout can cause further inflammation for many patients with an autoimmune condition. As always, it’s crucial to pay attention to how your body is feeling and respond accordingly.
How long does autoimmune flare-up last?
Depending on the severity of the natural stressor that is causing the flare-up, symptoms can last anywhere from a few days to several months. For some autoimmune disease sufferers who are not receiving treatment, symptoms of an acute flare-up may subside on their own without medical intervention after one or two weeks.
However, for others with unmanaged or more serious cases of autoimmune conditions, flare-ups may be an everyday struggle.
People with autoimmune diseases such as Hashimoto’s thyroiditis, psoriasis, and Lupus experience flare-ups that can last for several months or even years. For these individuals, natural therapies like diet and lifestyle changes are key to successfully managing the disease. These natural remedies often play a tandem role with conventional Western medicine interventions.
How do you prevent autoimmune reactions?
When people think of natural remedies they often think about herbs and supplements, but lifestyle choices like stress management techniques should be at the top of your list when attempting to decrease symptoms associated with an autoimmune flare-up. There’s no denying the powerful effect stress can have on your body and natural attempts to reduce stress tend to be quick-acting.
An integrative approach
As with other autoimmune disease symptoms, functional remedies that lower inflammation may not completely heal the condition but they do help manage symptoms and prevent flare-ups. Yoga has been shown as a natural remedy for autoimmune conditions like Hashimoto’s thyroiditis, while meditation has been shown to help the body handle natural stressors (6).

Supplements can also be helpful in decreasing inflammation caused by autoimmunity, such as:
- Glutathione
- Vitamin D
- Curcumin
- N-acetyl cysteine
- Probiotics
- Omega-3 fatty acids
Related: NAC: The Incredible Amino Acid for Your Lungs, Liver, and Longevity
Salt baths and meditation can also help support cellular health and support your immune system response to stress. Having healthy coping mechanisms in place is one important mediator of immune health which can decrease your autoimmune flare-ups.
Regular exercise
In one animal study, regular exercise has been shown to reduce the symptoms of autoimmune encephalomyelitis, a condition in which the immune system attacks the brain and spinal cord (7).
Traveling with Autoimmune Disease
Traveling is one of the most common times to experience an autoimmune symptom flare. If you’re traveling by car, bus or plane it’s best to plan ahead and learn how natural remedies can decrease your chances of an autoimmune reaction.
Planning a natural diet
When possible, eat foods that are easily digestible like minimally processed carbohydrates, and protein, and avoid very fatty or fried foods before and during any kind of travel. If you know there will be less than ideal food options available when you’re traveling, you can include some natural anti-inflammatory remedies to support your immune system if it’s already under stress.
foods before and during any kind of travel. If you know there will be less than ideal food options available when you’re traveling, you can include some natural anti-inflammatory remedies to support your immune system if it’s already under stress.
Include natural anti-inflammatory foods in your diet
Foods like ginger, turmeric, and garlic have been shown to decrease inflammation associated with autoimmune disease (8). If possible, pack some of these types of food when you travel.
Berries and other forms of fiber-rich veggies are also beneficial while traveling.
Read more: 6 Steps to Boost Your Immune System
Can vitamin D reverse autoimmune disease?
Vitamin D deficiency is associated with higher rates of autoimmunity, especially in women. A vitamin D deficiency and certain genetic variations significantly increase the risk for autoimmune diseases including multiple sclerosis, rheumatoid arthritis, alopecia areata (hair loss), and lupus (9).
It’s important to note that optimal vitamin D levels won’t protect you from developing autoimmunity, or from experiencing a flare-up, but many studies reinforce the fact that adequate vitamin D levels benefit the healthy function of immune cells, which in turn decreases the risk for autoimmunity.
This is why your functional medicine provider at CentreSpringMD will test for nutrient deficiencies when working with you to get your autoimmunity into remission.
Contact a qualified integrative medicine provider today and begin your journey to autoimmune remission.
What are the 7 most common autoimmune diseases?
Though there are more than 80 recognized types of autoimmune diseases to date, there are several which affect more individuals than others.
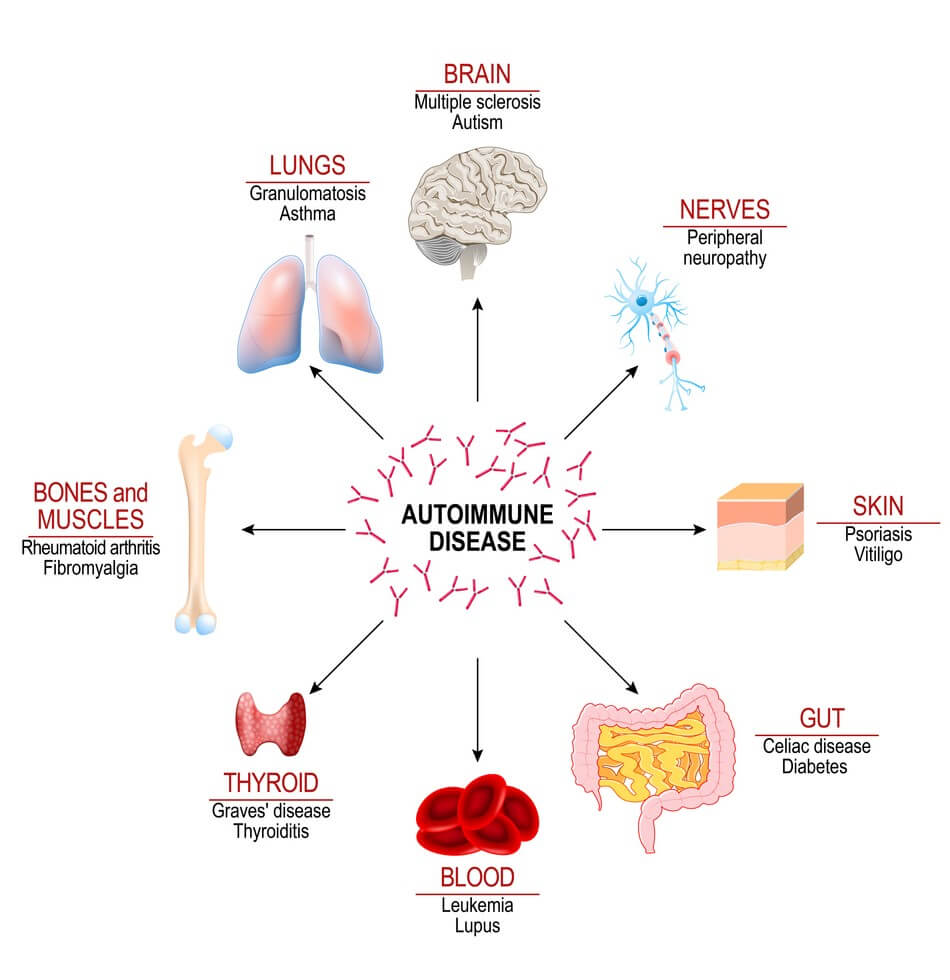
- Lupus is one of the most common autoimmune diseases, affecting women more than men, and is often misdiagnosed as other natural health problems like fibromyalgia or chronic fatigue syndrome.
- Hashimoto’s thyroiditis affects about 14 million Americans and is the most common cause of hypothyroidism or low thyroid.
- Type I diabetes, also known as insulin-dependent diabetes mellitus (IDDM), affects about five percent of Americans and usually appears in childhood or adolescence.
- Rheumatoid arthritis causes chronic inflammation to natural joints including your wrists, ankles, feet, and fingers which can lead to pain and disability.
- Multiple sclerosis, a disease that affects the brain and spinal cord which can cause problems from vision issues to muscle weakness or paralysis depending on where in your body the natural lesions are located.
- Psoriasis is an autoimmune condition affecting about seven million Americans with symptoms including itchy red patches of skin covered with natural scales that can appear anywhere on the body.
- Celiac disease (CD) is an autoimmune reaction to gluten, a natural protein found in common grains like wheat and rye which affects one out of every 133 Americans.
Managing Autoimmune Conditions with Integrative Medicine
For those who have been diagnosed with an autoimmune disease, it can be a constant struggle to manage the symptoms that come and go. There are many ways you can help yourself naturally on your own or by working closely with integrative providers like our team at CentreSpringMD. We offer in-depth support on how diet and lifestyle choices affect autoimmune flare-ups as well as traditional Western medicine options such as medication management and acupuncture therapy.
Contact us today if you’re interested in learning more about these treatment options!
Resources
- https://pubmed.ncbi.nlm.nih.gov/18190880/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7292717/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5097114/
- https://www.sciencedirect.com/science/article/pii/S1477893918300954
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6523821/
- https://pubmed.ncbi.nlm.nih.gov/21742277/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7818088/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5785894/
- https://bsd.biomedcentral.com/articles/10.1186/s13293-021-00358-3
